During my Monday morning troll of the medical literature I came across a paper in Nutrition Research showing that a semi-sort-of low-carb diet improves lipid profiles significantly better than does a low-fat diet.
The researchers who performed this study are a tad more enlightened that the normal run-of-the-mill lot we typically find doing this sort of work in that these folks looked at the lipid parameters most likely to be valid, if the lipid hypothesis is ever proven: triglycerides, HDL-cholesterol (HDL), and the number of small, dense LDL-cholesterol (LDL) particles.
Before we get into the study results, I want to take a bit to go over the problems that bedevil anyone trying to study diet. Macronutrients – fat, protein and carbohydrate – exert numerous effects on metabolism. And so do calories. The problem is in determining which of these variables causes the effect in question. If we place two groups of subjects on differing diets, one on a low-carb, high-fat diet and the other on a low-fat, high-carb diet, and we keep the calories the same in both groups, and we find that those subjects on the low-carb diet reduce their triglycerides, what does that tell us. Most of us will conclude that the reduction in carbs brought about the effect. But did it? It could just as easily have been the increase in fat.
What if in an effort to determine what’s going on, we decided to keep the fat the same in both groups and keep the calories the same, but to raise the protein intake in the lower-carb diet? If we find the same effect – the lowering of triglycerides – we can say that it’s probably the reduction in carbs, but we can’t say for sure because it could be that the increase in protein did the trick.
So we say, okay, we’ll keep the both the fat and the protein the same in both diets and simply lower the carbs in one diet and keep them high in the other. We do this and find that the triglyceride levels do indeed fall in the lower-carb diet. So that means that cutting carbs reduces triglycerides, right? Maybe, but we still can’t say for sure. Why? Because if we keep protein and fat the same in both diets and reduce carb in one and add carb in the other we end up with fewer calories in the low-carb diet. Protein is the same in both, fat is the same in both; but carbs are lower in one than the other, making the low-carb diet lower in calories. People can then justifiably say that maybe it is the reduced calories in the low-carb diet reducing the triglycerides and not the lowered carbs.
These are just some of the problems that come from manipulating the macronutrients and calories. There are other problems as well. If we give subjects diets and tell them to follow them on their own, then the specter of underreporting is involved. If we put subjects in metabolic wards, the expense of the study increases exponentially. And, contrary to what some people think about metabolic wards, these are not lock-down units, but are simply beds in a hospital designated for the study. As often as not, subjects in metabolic ward studies are free to go to their jobs during the day or roam around the hospital at will and have visitors. Subjects cheat during metabolic ward studies, and are probably less prone to admit it than they are on free-living studies. All in all, it’s difficult to get good reliable data from any kind of diet study. So, we’ve got to live with what we can get and make the best judgments we can.
The study we’re considering today has it’s own kind of problems. First, there aren’t a lot of subjects in the study, so differences in findings have to be large in order to reach statistical significance. And these subjects were randomized onto different diets, which, on the surface, seems like a good thing, but it may not be. Why? Because compliance could become an issue. Each of us has our own food likes and dislikes as well as our own ideas of what constitutes a good, healthful diet. If I love carbohydrates and consume a diet that is primarily carbohydrate, then I’m unlikely to pick up a book on low-carb dieting, and probably even less likely to go on a low-carb diet unless I become really convinced that such a diet is better for me. Same goes for someone who eats a lot of meat, cheese, eggs and other higher-protein, higher-fat foods. That person is unlikely to go on a low-fat, high-carb diet unless he/she becomes convinced of the superiority of that diet, and even then it would be difficult. Now if I or this other person are simply randomized onto a diet we don’t really enjoy and have no real motivation to follow, how likely are we to adhere to it faithfully? Not very, I would imagine.
If we allow subjects to select their own diets, that throws another kind of bias into the study because the subjects weren’t randomized. I’m droning on about all this simply to show how difficult good nutritional studies are to do because of all the variables involved. And no matter how a study is done, someone can poke holes in it for one or more of the reasons I mentioned above.
In the study we’re looking at today 23 subjects were randomized onto one of two diets for eight weeks: a low-carbohydrate diet or a low-fat diet.
The low-carb diet:
The goal of this diet was to have 15% of energy from CHO, 20% to 30% of energy from protein, and the remaining portion as fat (55%-65%) with saturated fat intake less than 10% of energy. The proportion of energy as fat is typical for a carbohydrate-restricted dietary plan. Subjects were given guidelines to avoid alcohol and simple sugars; CHO-rich foods such as breads, cereals, rice, pasta muffins, chips, pretzels, and crackers; select vegetables (potatoes, corn, peas, and dried beans); dairy foods; fruits; and fruit juices. No specific targets were imposed for the monounsaturated and polyunsaturated fatty acid intake or total calories.
The low-fat diet:
The low-fat dietary plan was based on the Therapeutic Lifestyle Changes portion of the Adult Treatment Panel Report III Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), JAMA 285 (2001), pp. 2486–2497.where subjects are advised to restrict calories, particularly from fat, to produce weight loss. Thus, a goal of 104.6 kJ/kg body weight was recommended. The targets as a percentage of energy were as follows: for CHO, 50% to 60% (with an emphasis on complex CHO); for protein, 15%; and for fat, 30% or less of energy with a reduced intake of transfatty acids and saturated fat intake below 10% of energy.
As you can see, the low-carb diet is not all that low-carb. Most rigid low-carb diets keep carbs in the 8 percent range, or about half of the 15 percent set for this low-carb diet.
In this study, calories were determined at the start. I have a little trouble believing the figures, which are 7095 ± 2520 kJ (calculates to 1695 ± 602 kcal) for the low-carb group and 7911 ± 3211 kJ (calculates to 1890 ± 767 kcal) for the low-fat group. This would mean that subjects randomized to the low-carb diet were on their normal diet consuming anywhere from 1093 to 2298 kcal and those randomized to low-fat were eating 1123 to 2657 kcal These are people who weighed in at around 200 pounds, so I find it unlikely that any of them were eating only 1093 kcal per day. In fact, I would bet that most of them were eating over 2700 kcal per day, so I don’t know where these figures came from. This brings up one of my real pet peeves. Why can’t researchers know when something doesn’t pass the smell test, and say, hey, wait a minute, something isn’t right here, then figure out what’s going on. So many of them simply enter the data without giving it a thought. Yeesh.
But, that misstep aside, I think we can pull some interesting data from this study. These subjects were given instruction in one of two diets, a handful of meal plans, and sent on their way for eight weeks. Despite each subject’s also receiving dietary instruction on an alternating weekly basis throughout the study (via telephone, I assume), these people were regular people trying to follow a diet, much like people who buy diet books. It’s cheering to learn that even doing it this loosy goosey, not-very-controlled, way that the subjects on the low-carb diet did better in terms of their lipid changes.
Here is Table 2 from the study:
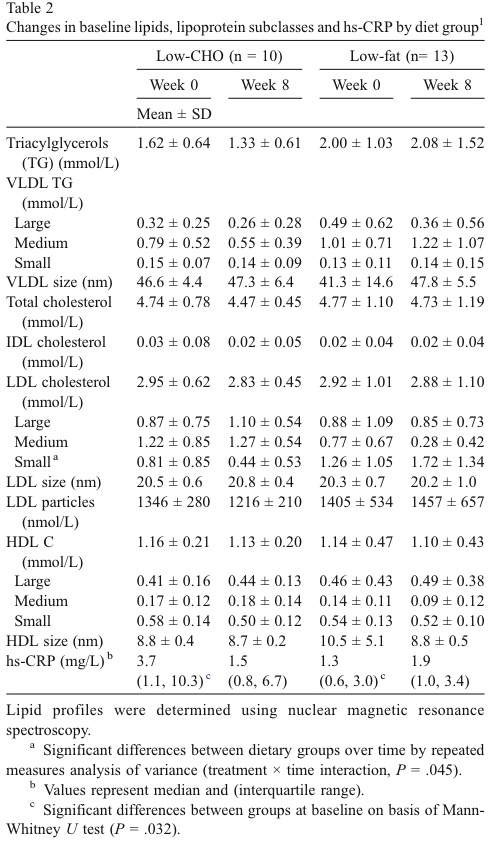
If you live in the United States, these numbers won’t make much sense to you because they are in mmol/l, which is a measurement used everywhere but the US. To convert to mg/dl, the US system, multiply the triglyceride values by 89 and the LDL and HLD values by 39.
It’s interesting to note that these subjects had triglyceride levels and LDL levels before starting the two diets that were not elevated by any means. The low-carb group had starting triglycerides of 144 mg/dl and starting LDL levels of 115 mg/dl. The low-fat group had triglycerides of 178 mg/dl and LDL of 114 mg/dl. Even lipophobic physicians wouldn’t consider these values as worrisome.
After eight weeks, the subjects on the low-carb diet saw their concentrations on small, dense LDL particles fall by almost half whereas those on the low-fat diet watched theirs rise from 49 mg/dl to 67 mg/dl, a 37 percent increase. If any single lipid parameter truly corresponds to a real risk for the development of heart disease, it is this one. And it’s nice to learn that a less-than-rigid low-carb diet – even if followed loosely by people who aren’t all that motivated – halves it. Just think what would happen if these subjects really dug in and followed a more rigid low-carb diet. And these subjects didn’t have bad numbers to begin with. Imagine what might have happened had they had elevated levels of small, dense LDL particles.
Don’t ask me why, but these researchers, for whatever reason, chose to limit the saturated fat on the low-carb diet to less than 10 percent of calories. I suspect that if the saturated fat intake had been higher, we would have seen an even more pronounced lowering of the small, dense LDL. I guess even somewhat enlightened researchers just can’t bring themselves to recommend saturated fat, even for a short-term study.
As you can see from Table 2, C-reactive protein (a measure of total body inflammatory load) was substantially lowered in the low-carb group while it increased in the low-fat group. But the figures didn’t reach statistical significance due to the small number of subjects, so we can’t really make a claim here. But it does give us the tantalizing hope that were this group of subjects larger, we would have seen the same difference. I would bet money that we would.
So, we have yet one more study to add to our growing pile showing the superiority of the low-carb diet for all sorts of good things. In this case, the improvement of the atherogenic lipoprotein profile. Use it the next time someone hits you with the old ‘that diet is clogging your arteries’ nonsense.

Thank you Dr. Eades for such detailed reporting on these studies. I can’t believe you just give all of this information away. Even though I’m sold on low-carb through personal experience, I feel the need to buy your new books just to pay you back for all of the advice and guidance you have given through your blog and in previous books. I hope you make lots of money on the new book. You deserve it for all of the value you have given me and my family in better health.
Cheers,
Guy
Why stop with buying just one book? I would suggest several hundred at least. 🙂
Just kidding. Thanks for the kind words.
Cheers–
MRE
“I can’t believe you just give all of this information away. ”
Hey, don’t give him any ideas! 😉
Like commenter Cheerwino above, I, too, am very grateful for the knowledge I’ve gained about my health, primarily from you and also from Dr. Wm. Davis. But I also find it kind of sad that I am in better health because of doctors whose blogs I read on the internet than from the advice I receive from my PCP. She’s useful for prescribing an antibiotic when I get the occasional sinus infection, but she’s not in the know at all about nutrition. Come to think of it, because of the reading I do here and elsewhere, I probably know more about nutrition than she does, and that’s a sad commentary on our medical system, too. Especially considering how much she bills me and my insurance company to dole out advice that would make me fatter and sick if I followed it.
What a glorious day it was when I vowed never to eat another no fat/reduced fat food product ever again!
If you had several hundred different books of even partial (new) value of the others I’ve read, I would buy them. I’m glad you have a blog to keep updated info available while you write new books.
I wonder if giant cell arteritis is actually produced by low fat diets? You see it in the elderly where often their family physician tells them to stay on one to lower their cholesterol.
I’ve never treated much giant cell arteritis, so I don’t have a lot of hands-on experience with it. Your hypothesis sounds plausible, however. Have you put pts with GCA on low-carb diets and seen improvement?
Best–
MRE
Some of the issues you addressed in experimentation arise from studying one factor at a time (OFAT). These issues can be resolved with a proper design of experiment (DOE) approach and multiple factors can be studied at one time. I’ve often wondered why some postdoc in a lab somewhere hasn’t pulled in all the data from existing experiments and studied these with just a few factors in a DOE. It is labor intensive, but appropriate for young researchers with more time on their hands.
Also, I didn’t catch if the above diets were considered hypo caloric. My experience with the low carb diet, when trying to maintain weight, was the opposite of that described above. Everything went up, but my “ratio” slightly improved.
I imagine it would be extremely labor intensive. And difficult, I would think.
If you can believe the data, it would appear that these diets were hypocaloric. Although I’m not sure I believe the data on energy intake.
As to your experience, I’ll bet if you had measured LDL particle size concentration, you would have found it decreased.
Cheers–
MRE
Why not do these types of studies on prisoners? They are already in a “ward” of sorts, at taxpayers expense. I imagine most prisons/jails limit the amount of items brought in from visitors, so it would be fairly easy to control food brought in. And those who aren’t hard core criminals might be able to get a reduced sentence for cooperating with the study.
And since their room & board is already paid for (by you and me), it would be less expensive for the researchers to carry out such a study. Who knows, the prisoners might come out of the study healthier, and better able to function when they do get out of prison.
It’s just a thought, anyway.
I agree. Many experiments have been done with prisoners, the most famous of which (nutritionally, at least) are the overfeeding studies done 30 years ago by EA Sims in the Vermont prison system.
Dr. Eades
I found some studies on the role of insulin in atherosclerosis that I thought you would find of interest:
http://www.ncbi.nlm.nih.gov/pubmed/1505650
http://www.ncbi.nlm.nih.gov/pubmed/8596596?ordinalpos=7&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
http://www.ncbi.nlm.nih.gov/pubmed/17760500?ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
http://jama.ama-assn.org/cgi/content/full/279/24/1955
http://www.ncbi.nlm.nih.gov/pubmed/9167103?ordinalpos=5&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum
I wasn’t able to track down an older article I was looking for though:
http://www.ncbi.nlm.nih.gov/pubmed/4183909
Thanks
Hi Freddy–
Thanks for the links. I’m intrigued by the very last one by Stout; I’ll see if I can dig it out. These are but the tip of the iceberg of studies showing a correlation between hyperinsulinemia and heart disease. What I would really like to see are studies showing that atherosclerosis diminishes with an insulin-lowering diet.
Cheers–
MRE
P.S. I went ahead and pulled the Lancet paper. Pretty interesting.
Here is the author’s abstract:
Summary: Rats given sodium [14C]-1-acetate and
insulin intravenously were killed 1 hour
later. Radioactivity levels in cholesterol in aortic tissue
were significantly higher than in rats given labelled
acetate alone. Levels in serum-cholesterol were not
significantly different, nor were aortic-tissue levels
when [14C]-4-cholesterol was given with or without
insulin. The result suggests that insulin stimulates
cholesterol synthesis in the aortic wall.
Excellent post and an explanation why the medical community for cardiac health is still concerned about the level of sat fat in the diet. Nevertheless, my own recent experience in a visit to a cardiologist was very enlightening and perhaps may be evidence of of changing veiws in the medical community. Due to a bad family history of heart attack- brother(non smoker) at age 52, and father(smoker) in young 60’s he is concerned based upon that, an IMT score higher than i should have for my age(57) and a small particle count of 1800 almost all of which are small dense( trigllycerides are 37) he thinks it needs to be addrressed. His prescription is a low carb diet,(he said no Ornish type diet- high carb as that is not the way to go!) but he is concerned about having to much sat fat in diet. He said to eliminate all starches, sugars,etc and eat fruits veggies and lean animal protein. He does want me on a 10mg statin which i will do and to add fish oils and baby aspirin and come back in 90 days for retesting to see if the diet can change the particle types.
So, while not wholly subscribing to low carb, he is partially in the camp. Will see if the diet.
Thank you because i mentioned to him i was aware of low carb benefits (which i learned from this site) regarding particle size and he was surprised i knew anything about the topic.
I’m glad to see your doc is at least leaning in the right direction. I don’t think, however, that statins have been shown to reduce the levels (or change the ratio) of small, dense LDL particles. Make sure you take some CoQ10 (I would say at least 200 mg/day) if you’re going on even a small dose of statins.
Senor Eades is seemingly a good egg/decent bloke/grooming primate and not like those shiy-sters who have a paid for blog which is surely akin to a fan club basically which says more about the person that owt else.
And its a smart thing as the readers seem to have more ‘brand’ loyalty to a person who gives of themselves than money grabbing oiks and thus i’d wager most readers of this blog might buy the new Eades book with or without a cheesy picture !
All hail Les Eades
Simon, Simon, Simon. What can I say?
Thanks for your support. I appreciate it.
Cheers–
MRE
A couple of things:
1. Tierney just posted Part I of a two part response to Gary Taubes’ take on the diet study on his blog – Ornish’s comments are about what one would expect from him.
2. Any thoughts on this study (http://jama.ama-assn.org/cgi/content/abstract/298/3/299) from a year ago about the predictive value of NONfasting triglyceride levels?
Hey Michael–
I was just posting on Ornish’s comments to Taubes when your comment came in.
I read this study when it came out. It is intriguing and many researchers are starting to look at post-prandial lab values (as opposed to fasting) to discover how the body handles various caloric loads. Although the study raises some interesting issues, it is still an epidemiological study, not a controlled, randomized, prospective study, and, as such, is valuable only for formulating hypotheses.
Cheers–
MRE
Dr.
Well, here’s my own lipid panel after about a year on low-carb, high fat.
http://www.honestylog.com/root/2008/07/lipid-pannel.html
Last time it was checked, about three years ago, TRI was around 150ish and HDL about 60ish. How often do you see an HDL of 106 or higher, and how often an HDL higher than LDL?
Anyway, that’s my anecdote.
One other question, however. my TSH came in at 16, where the normal range is like 4-6 or something. The doc wants me to go on thyroid, but in the last year I’ve lost 50 pounds of fat and gained 20 pounds of lean mass through brief but intense resistance training. I feel great, never tired, and am getting leaner toward my goal of 10% BF.
So, the question is, how can I research this to see if I really need the meds or not? My concern is that “typical” really means “typical for a grain eater,” in which case those norms would be non-sequitur to my individual case.
Nice lab results. Thanks for providing for all to see.
I wouldn’t think of going on thyroid hormone until I had a more thorough thyroid work up. The elevated TSH level could simply be a lab error. Get it rechecked, and an entire thyroid profile along with it. And if my thyroid profile looked a little hypothyroid, I would first take some iodine (you can get Iodoral online) and see what happens. (You can also do an iodine retention test that will tell you if you are iodine deficient or not.) If I ended up having to take thyroid, I would take Armour Thyroid, not levothyroid, the most commonly prescribed thyroid hormone.
Dr. Eades
With regard to your request to finding studies on low-carb diets and heart disease, even better results can be found! There is a doctor in Poland named Jan Kwasniewski who practices with what is called Optimal Nutrition that mandates the consumption of a lot of animal fat. Daily food intake is supposed to make the proportion 1 : 2.5-3.5 : 0.8 grams of protein, fat, and carbs per kilogram of bodyweight. Thus a adult male may consume 60 grams animal protein, 180 grams animal fat, 50 grams carb (preferably starch). With this diet he has been able to reverse not only heart disease, but also cancer, diabetes, joint disease and osteoporosis. It has even been able to halt the progression of ALS and leads to a certain level of recovery (though not a complete one in longstanding cases). Several doctors in Europe have claimed to have cured AIDS with this diet, though this has been hearsay so far.
Unfortunately, quite a lot of his research is in Polish and is denied by most Polish authorities (because it has too much fat and cholesterol!). Some of his papers can be found on his website though at:
http://translate.google.com/translate?hl=en&sl=pl&u=http://www.dr-kwasniewski.pl/&sa=X&oi=translate&resnum=4&ct=result&prev=/search%3Fq%3Djan%2Bkwasniewski%2B.pl%26hl%3Den%26sa%3DG
It is worth reading through some of his papers (use Google translate), especially those on heart disease. According to him, glucose is converted inside the arterial wall to triglycerides and then into cholesterol in order to provide oxygen and fats to these “undersupplied” organs in certain nutritional situations. Here is one good article:
http://translate.google.com/translate?hl=en&sl=pl&u=http://www.dr-kwasniewski.pl/&sa=X&oi=translate&resnum=4&ct=result&prev=/search%3Fq%3Djan%2Bkwasniewski%2B.pl%26hl%3Den%26sa%3DG
Thanks
Thanks for the links. I couldn’t get the papers to come up, however, translated or not.
Cheers–
MRE
Just when you thought it was safe to declare victory…
“Lowering Cholesterol Early In Life Could Save Lives”
http://www.sciencedaily.com/releases/2008/08/080804190637.htm
The statinators hit back… Start ’em early! Why not just spike their baby formula with Pravastatin?
Jesus is still weeping methinks.
This is a paper from Daniel Steinberg, who is a statinator of renown and is heavily vested in the lipid hypothesis. I wouldn’t put a lot of stock in it.
Here’s an interesting study I just came across that shows how growth hormone can affect glucose paths.
Growth Hormone Treatment For HIV Patients Improves Abdominal Fat, But Worsens Glucose Level
ScienceDaily (Aug. 3, 2008) — For human immunodeficiency virus (HIV)-infected patients with treatment-related abdominal obesity and growth hormone deficiency, receiving low-dose growth hormone resulted in improvement in fat and blood pressure measurements but worsened glucose levels, according to a study in the August 6 issue of JAMA, a theme issue on HIV/AIDS.
The researchers found that abdominal fat decreased significantly in the GH group compared with the placebo group, with a percentage change in the GH group of −8.5 percent and −1.6 percent in the placebo group. Trunk-to-lower extremity fat ratio and trunk fat also decreased in the GH group compared with the placebo group.
Triglycerides and diastolic blood pressure (BP) levels improved with GH, while the change in systolic BP was not statistically different compared with placebo. Total cholesterol and high density lipoprotein (HDL) cholesterol levels were unchanged between the two groups. GH increased glucose levels during glucose tolerance testing, however long-term indices of glucose, hemoglobin A1c (the substance of red blood cells that carries oxygen to the cells and sometimes joins with glucose), were not different between the groups.
http://www.sciencedaily.com/releases/2008/08/080804100520.htm
Dr. Eades,
I’ve been waiting for 2 days for a comment I wrote in your
“weight-loss/low-carb-and-calories-2” column to be “approved.” At first I thought it might be because you were busy and unable to get to comments to your articles, but then I see that you’ve been approving them in this topic.
Can you please approve my comment in the other column — even though, basically, it takes issue with your own comments on the topic — or should I re-post those comments here?
Best wishes,
Ellen
Hi Ellen–
I will post it momentarily. It was a long comment that I didn’t totally disagree with, but I wanted some time to reflect on it and maybe look up a reference or two before I made my comment to it.
I’ll be happy to post it and let others comment.
Cheers–
MRE
I am just chalking up two years as a low-carber. I had a cholesterol test last week and just got my results:-
Serum Cholesterol 4.8%
Triglycerides: 0.5
My weekly diet includes a whole chicken (including the skin), a couple of steaks (including the fat), 8 rashers of bacon (fried in the chicken fat saved from the fowl above), one lamb’s liver and upto 12 eggs a week. I will also eat about 8 tins of either pilchards/tuna/mackerel/sardines a week. My body fat is well under 10%.
I do not eat whole grains, pasta, rice, cereal, bread, potatoes, pastries or any goods containing refined-carbohydrate.
Your blog is one of the main sources that gave me the confidence to go down this dietary route. Many thanks.
Chris
PS I’m looking forwards to the new book!
I’m glad you’re enjoying the blog. Thanks for your support.
Cheers–
MRE
“Here’s an interesting study I just came across that shows how growth hormone can affect glucose paths.”
I’ve had some interesting personal experience in this area. First, I do lots of stuff to promote GH release, as I’ve not merely wanted to “lose weight,” but to lose fat and gain muscle. As I said in my last comment, I’m at 50 pounds fat loss, 20 pounds lean gain for a net loss of 30.
To promote GH release I train briefly (30 minutes x2 per week) but very intensely (heavy weight, little to no rest between sets). Lots of leg and back work, i.e., the big muscles where most GH stimulation comes in. Also: fasting. And: sleep. I also do all this in combo.
My Ac1 is at 4.8, which is right at the low, yet it is not uncommon to have a random blood glucose of 110ish. In one self-experiment, I had gone 30 hours fasting when I tested: 85ish. Went to the gym, did my normal workout, then tested as soon as I got home, which was about 45 minutes after the completion of my workout. So, I’d not eaten in about 31 hours, and with a heavy workout right at the end. Random Blood Glucose came out near 110.
I had always thought this was simple temporary insulin resistance from the stress of the workout, as well as fat burning and gluconeogenesis, but perhaps the GH also plays a direct role. Anyway…
Dr, to clarify from my last, it’s not a lab error. I was first diagnosed about 5 years ago and had been on 125MCG levothroid all this time. Right around the last holidays, after about three months of really low carb and really high fat, I had lost about 20 pounds of fat, gained 10 pounds leans for a net of 10. I felt great, this is when I began employing the intermittent fasting, and I just stopped taking the thyroid meds. My weight (fat) loss really accelerated. Now, maybe that’s all or mostly do to the fasting, but it does seem odd to me. At any rate, I have no intention of going back to the meds until I drill down and find out as best I can what’s going on.
Good idea on the drilling down. If you do go on meds, it’s been my experience that Armour Thyroid (dessicated thyroid) is much better than levothyroid. Talk your doc into letting you give it a go.
To Richard with questions about thyroid:
Many, if not most, doctors think that TSH IS a full thyroid panel. Be sure to insist on Free T3 and Free T4 tests, as well as the repeat TSH. If your doctor won’t prescribe Armour thyroid, you can try synthetic T4 (several brand names, all equivalent) and synthetic T3 (only one brand – Cytomel). It requires more testing to get the Free T3 and T4 levels in similar parts of the normal ranges. I feel better when both are in the top 1/3 of the normal range for each. Please note that total T4 and T3 levels are not the same as Free levels (that’s what is actually circulating and available for use in your tissues).
Thanks Dr, Eades for all your hard work getting real information about nutrition out for us, instead of us having to try and decipher the non-sense the media presents.
Dr. Eades,
My liver function tests were elevated because of eating a lot of butter & drinking 4 glasses of wine per night over a 10 year period. I have since stopped the wine and am on the Promedis liquid low carb diet to hopefully lose about 35 pounds and am under an Endocronologist’s supervision. This includes 2 Promedic drinks per day and 1 Promedic bar and a low fat (lean meat or fish or poultry, 3-4 oz per evening meal, plus veggies). Do you think that this diet will correct my liver function tests and bring them back to normal. I plan to not drink any alcohol in the future. Thank you for any info you can give me.
Sharon
It’s been my experience with many, many patients that liver function tests normalize fairly quickly once they started following a low-carb diet, especially if they decreased their consumption of alcohol as well. I don’t think your liver function tests were abnormal because of the butter – I suspect it was because of a number of other factors. Studies have shown that increasing saturated fat intake and decreasing vegetable oil intake helps to improve liver function.
Dr. Eades:
First-time post from a long-time devotee of your ProteinPower plan, on which I’ve lost nearly 35 pounds and have kept that weight off for nearly 6 years now. I’d like to take my weight down another 20 pounds, which would bring me to my best-health weight of 175.
My question pertains to your ending comment in the post above: “Studies have shown that increasing sat fat intake and decreasing veg oil intake helps improve liver function.”
I have no reason to believe that my liver function is impaired, but I’d like to ask your opinion of organic COCONUT OIL intake and its role (as a largely-saturated fat) in lipid profiles and overall health. My family and I love the taste when we cook with it, but there has always been a cloud over our use of that oil because of the mixed opinion about lipid effects. Anything you might add will be much appreciated. All the best…Don in CT
I love organic coconut oil. That is MD’s fat of choice to cook with. It contains a lot of good immune enhancing short-chain fatty acids that are hard to get from other sources, and isn’t damaged in the cooking process. Go for it.
Dear Dr,
I am a regular reader of your blog and follow low carb diet (40g of carbs every day).
While I come across the normal BG levels, what is the accepted normal triglyceride levels if someone is in low carb? I am referring about the postprandial (PP) levels (2 hours after food)?
Mine was 283 PP when the Dr tested once and after that I have been tested only fasting. Both the time it was 95 and 119(last time). All other lipid parameters are at normal levels (both during fasting and PP).
Thanks
Venkat
I really don’t know what the postprandial levels should be. It depends a great deal on what the meal was. I typically check fasting levels, and in patients on low-carb diets those are usually under 100 mg/dl.
Low Carb diet like low GI, attempts to regulate the rise in blood glucose levels after eating, which can assist in keeping you full longer.
But isn’t low carb also low fiber and can cause constipation?
Not really. The increased fat content of the diet prevents the constipation. The more I study it, the less fiber I think we really need.